Periodontal Disease
Don't wait until it's too late

If you have been diagnosed with periodontal disease, you are not alone. Many others have the same problem. Finding the disease is the first step in preventing tooth loss.
What is Periodontal Disease?
Periodontal disease is an infection that affects the tissues and bone that support teeth.
Healthy gum tissue fits like a cuff around each tooth. When someone has periodontal disease, the gum tissue pulls away from the tooth. As the disease worsens the tissue and bone that support the tooth are destroyed. Over time teeth may fall out or need to be removed. Treating periodontal disease in the early stages can help prevent tooth loss.
Can gum disease cause health problems beyond the mouth?
In some studies, researchers have observed that people with gum disease (when compared to people without gum disease) were more likely to develop heart disease or have difficulty controlling blood sugar.

Other studies showed that women with gum disease were more likely than those with healthy gums to deliver preterm, low birth weight babies. But so far, it has not been determined whether gum disease is the cause of these conditions.
There may be other reasons people with gum disease sometimes develop additional health problems. For example, something else may be causing both the gum disease and the other condition, or it could be a coincidence that gum disease and other health problems are present together.
More research is needed to clarify whether gum disease actually causes health problems beyond the mouth, and whether treating gum disease can keep other health conditions from developing. In the meantime, it's a fact that controlling gum disease can save your teeth – a very good reason to take care of your teeth and gums.
What causes periodontal disease?
Our mouths are full of bacteria. These bacteria, along with mucus and other particles, constantly form a sticky, colourless "plaque" on teeth. Brushing and flossing help get rid of plaque. Plaque that is not removed can harden and form calculus or "tartar" that brushing doesn't clean. Only a professional cleaning by a dentist or dental hygienist can remove tartar. The longer plaque and tartar are on teeth, the more harmful they become. The bacteria cause inflammation of the gums that is called "gingivitis". In gingivitis, the gums become red, swollen and can bleed easily.
Gingivitis is a mild form of gum disease that can usually be reversed with daily brushing and flossing, and regular cleaning by a dentist or dental hygienist. This form of gum disease does not include any loss of bone and tissue that hold teeth in place.

When gingivitis is not treated, it can advance to "periodontitis" (which means "inflammation around the tooth"). In periodontitis, gums pull away from the teeth and form spaces (called "pockets") that become infected. The body's immune system fights the bacteria as the plaque spreads and grows below the gum line. Bacterial toxins and the body's natural response to infection start to break down the bone and connective tissue that hold teeth in place. If not treated, the bones, gums, and tissue that support the teeth are destroyed. The teeth may eventually become loose and have to be removed.
Are you at risk?
A risk factor is something that increases your chance of getting a disease or condition. Risk factors for gingivitis include:
-
Inadequate brushing and flossing
-
Stress
-
Clenching teeth together or grinding teeth
-
Poor nutrition
-
Diabetes
-
Breathing through the mouth
-
HIV and AIDS
-
Improper bite
-
Advancing age
-
Pregnancy
-
Birth control pills
-
Family members with gum disease
-
Sex: male
-
Poorly fitting dentures
-
Some medications taken for High Blood Pressure , Coronary Artery Disease , and Depression
-
Some seizure medications
-
Drinking alcohol
-
Smoking
The stages of periodontal disease

In a healthy mouth the gingiva (gum tissue), periodontal ligament and bone anchor teeth firmly in place. As gingivitis develops toxins and other plaque by-products irritate the gums, making them tender, swollen and likely to bleed easily.
Periodontitis occurs when plaque by-products lead to the destruction of the tissues that anchor the teeth in the bone. As the disease progresses, pockets form which allow more plaque to collect below the gum line. Tooth roots are exposed and may become at risk of decay and sensitive to cold and touch. As the disease progresses, the teeth become loose and the presence of pus in the deep pockets can lead to pain, swelling and a foul odour. Removal or loss of teeth may occur.
Types of periodontal diseases
Gingivitis
Gingivitis is the mildest form of periodontal disease. It causes the gums to become red, swollen, and bleed easily. There is usually little or no discomfort at this stage. Gingivitis is often caused by inadequate oral hygiene. Gingivitis is reversible with professional treatment and good oral home care.
Periodontitis
There are many forms of periodontitis. The most common ones include the following:
-
Aggressive periodontitis occurs in patients who are otherwise clinically healthy. Common features include rapid attachment loss and bone destruction and familial aggregation.
-
Chronic periodontitis results in inflammation within the supporting tissues of the teeth, progressive attachment and bone loss. This is the most frequently occurring form of periodontitis and is characterized by pocket formation and/or recession of the gingiva. It is prevalent in adults, but can occur at any age. Progression of attachment loss usually occurs slowly, but periods of rapid progression can occur.
-
Periodontitis as a manifestation of systemic diseases often begins at a young age. Systemic conditions such as heart disease, respiratory disease, and diabetes are associated with this form of periodontitis.
-
Necrotizing periodontal disease is an infection characterized by necrosis of gingival tissues, periodontal ligament and alveolar bone. These lesions are most commonly observed in individuals with systemic conditions such as HIV infection, malnutrition and immunosuppression.
How do I know if I have gum disease?
Symptoms of gum disease include:
-
Bad breath that won’t go away
-
Red or swollen gums
-
Tender or bleeding gums
-
Painful chewing
-
Loose teeth
-
Sensitive teeth
-
Receding gums or longer appearing teeth
Any of these symptoms may be a sign of a serious problem, which should be checked by a dentist. At your dental visit the dentist or hygienist should:
-
Ask about your medical history to identify underlying conditions or risk factors (such as smoking) that may contribute to gum disease.
-
Examine your gums and note any signs of inflammation.
-
Use a tiny ruler called a "probe" to check for and measure any pockets. In a healthy mouth, the depth of these pockets is usually between 1 and 3 millimeters. This test for pocket depth is usually painless.

Your dentist may also:
-
Take an x-ray to see whether there is any bone loss.
-
Refer you to a periodontist. Periodontists are experts in the diagnosis and treatment of gum disease and may provide you with treatment options that are not offered by your dentist.

Left: Healthy gums and bone levels seen both in the mouth and on x-ray
Right: Bone loss seen in periodontitis, both in the mouth and on x-ray
How is gum disease treated?
The main goal of treatment is to control the infection. The number and types of treatment will vary, depending on the extent of the gum disease. Any type of treatment requires that the patient keep up good daily care at home. Your dentist may also suggest changing certain behaviours, such as quitting smoking, as a way to improve treatment outcome
Scaling and Root Planing
Scaling and root planing is a careful cleaning of the root surfaces to remove plaque and calculus (tartar) from deep periodontal pockets and to smooth the tooth root to remove bacterial toxins. Scaling and root planing is often followed by adjunctive therapy such as local delivery antimicrobials and host modulation, as needed on a case-by-case basis.
Medication
Your dentist may recommend medicines to help control infection and pain, or to aid healing. These medicines could include a pill, a mouthrinse or a substance that the dentist places directly in the periodontal pocket after scaling or root planning. Your dentist may also stress the need to stop using tobacco and to control any related systemic disease, like diabetes.
Surgical Treatments


Flap Surgery
Surgery might be necessary if inflammation and deep pockets remain following treatment with deep cleaning and medications. Your dentist or periodontist may perform flap surgery to remove tartar deposits in deep pockets or to reduce the periodontal pocket and make it easier for the patient, dentist, and hygienist to keep the area clean. This common surgery involves lifting back the gums and removing the tartar. The gums are then sutured back in place so that the tissue fits snugly around the tooth again. After surgery the gums will heal and fit more tightly around the tooth. This sometimes results in the teeth appearing longer.
Bone and Tissue Grafts
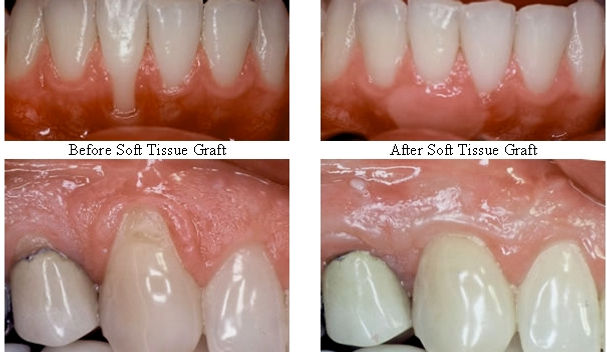
In addition to flap surgery, your periodontist or dentist may suggest procedures to help regenerate any bone or gum tissue lost to periodontitis. Bone grafting, in which natural or synthetic bone is placed in the area of bone loss, can help promote bone growth. A technique that can be used with bone grafting is called guided tissue regeneration. In this procedure, a small piece of mesh-like material is inserted between the bone and gum tissue. This keeps the gum tissue from growing into the area where the bone should be, allowing the bone and connective tissue to regrow. Growth factors – proteins that can help your body naturally regrow bone – may also be used. In cases where gum tissue has been lost, your dentist or periodontist may suggest a soft tissue graft, in which synthetic material or tissue taken from another area of your mouth is used to cover exposed tooth roots.
Since each case is different, it is not possible to predict with certainty which grafts will be successful over the long-term. Treatment results depend on many things, including how far the disease has progressed, how well the patient keeps up with oral care at home, and certain risk factors, such as smoking, which may lower the chances of success.
Care after treatment
Once your periodontal treatment is complete, your dentist may recommend more frequent check ups. Regular dental visits and deep cleanings are important to keep periodontal disease under control. In some cases, your appointments may alternate between your general dentist and a periodontist.
How can I keep my teeth and gums healthy?
-
Brush your teeth twice a day (with a fluoride toothpaste).
-
Floss regularly to remove plaque from between teeth. Or use a device such as a special brush or wooden or plastic pick recommended by a dental professional.
-
Visit the dentist routinely for a check-up and professional cleaning.
-
Don’t smoke.
How to find us
Modern Dentistry
Level 1 City Walk Centre
City Walk
Civic
Canberra
ACT 2601
Above King O'Malleys Pub
Work: 02 6247 8400
Opening Hours
Modern Dentistry
Monday - 8:30 am - 5:30 pm
Tuesday - 8:30 am - 5:00 pm
Wednesday - 8:30 pm - 5:30 pm
Thursday - 8:30 am - 5:30 pm
Friday - 8:00 am - 3:30 pm
Saturday - Closed
Sunday - Closed
